The Quick Rundown:
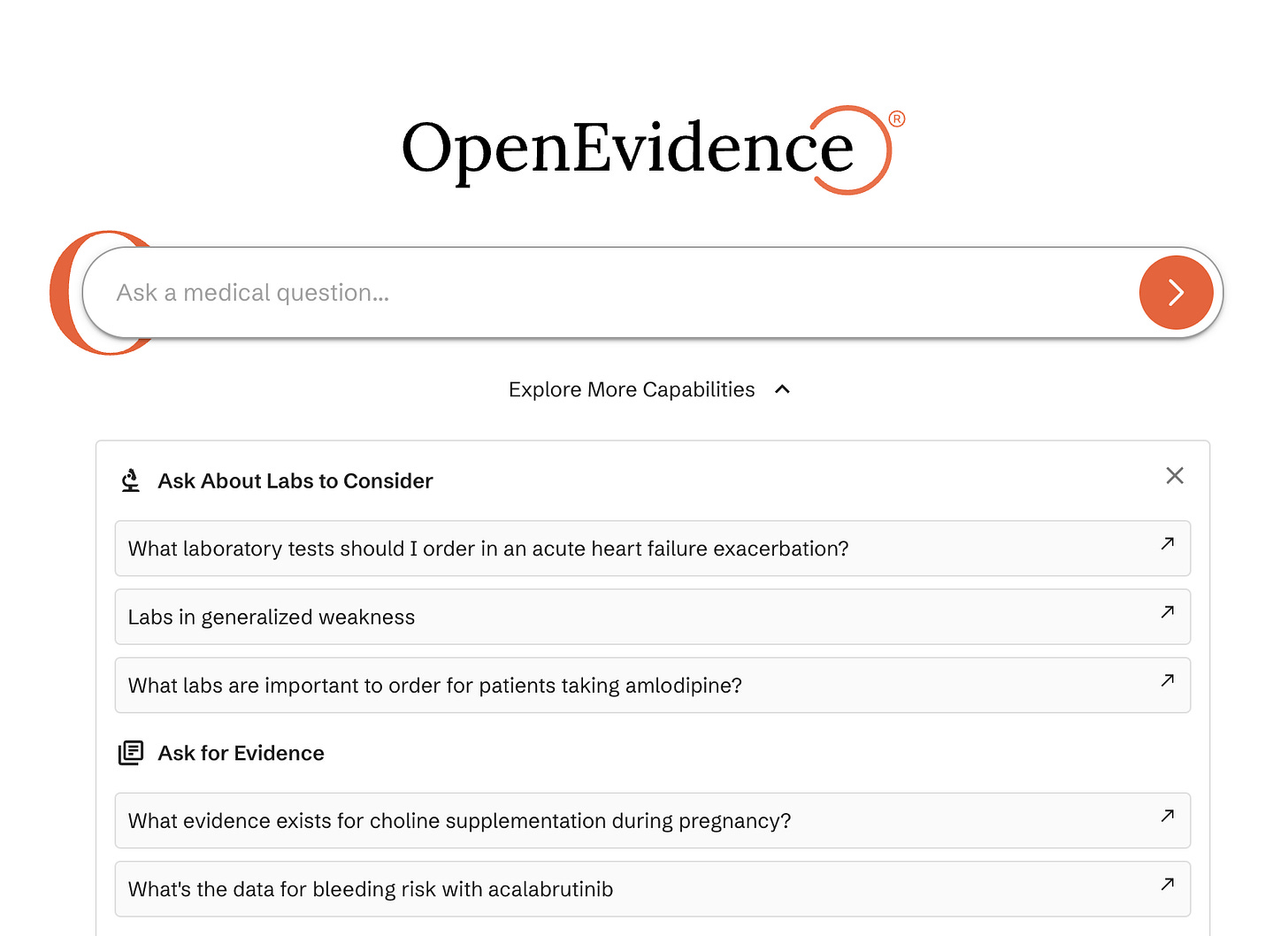
OpenEvidence enables doctors to make high-stakes clinical decisions at the point of care via an AI model trained exclusively on medical content from journals including The New England Journal of Medicine.
With 35,000 physicians registering each month, OpenEvidence is on track to have 50% of US doctors using their platform by the end of the year, potentially making them the fastest-growing healthcare company in history.
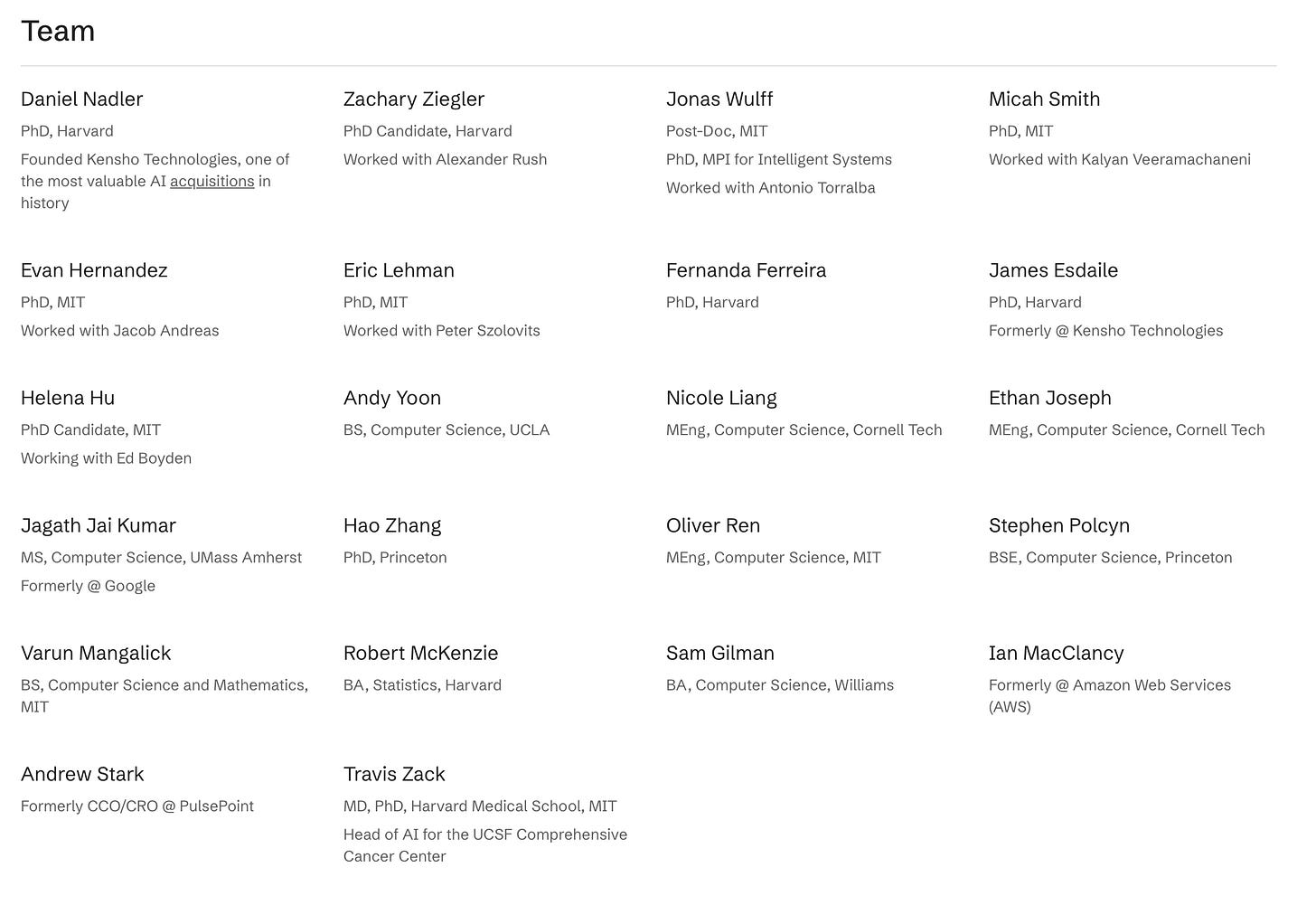
They’ve just raised a $75M Series A led by Sequoia and are hiring engineers – send over an email to engineering@openevidence.com.
This is “Startups to Join” – a blog for engineers and designers to discover early-stage startups that are reimagining industries and on the path to becoming enduring companies. Whether you’re looking for the next unicorn to join or just curious about what VCs are investing in, subscribe below to keep updated.
The Biggest Company In The World Will Be a Health Tech Company
Around two years ago, just before the launch of ChatGPT, I worked on a thesis with the podcast team at a16z about why the biggest company in the world would be a health tech company. At that time, a few shifts were happening which meant that it was a unique moment in time to build a health tech startup:
First, the Cures Act, No Surprises Act, and the PRICE Transparency Act went into effect. These regulations gave Americans the ability to access their health and insurance data via an API call and they reduced surprise medical bills.
Second, COVID meant that traditionally centralized care delivery services started to move to community-based and virtual settings, unbundling the hospital and changing doctor-patient interactions.
Third, alongside the shift in the delivery of care, there was also a growing push to move from the typical fee-for-service revenue model to new variations of value-based pricing models.
These changes meant that the door to innovating in healthcare – a category that has been notoriously difficult to build in – was starting to open.
But, while this thesis got many things right, one thing it didn’t fully appreciate was how hard it is to overcome misaligned payor and provider incentives, the long sales cycles, and the tiny budget that providers actually have because of their low margins. This meant that despite the significant inefficiencies that existed in back office workflows – e.g. for every $1 a hospital makes, $0.25 is spent on the administrative costs required to collect it – very few startups achieved significant distribution.
Why Now
Despite these failed attempts to innovate in healthcare, AI has now opened up a new window of opportunity. Instead of dealing with long sales cycles and product/data integration challenges, startups can now provide immediate value with low friction.
One area where AI is perfectly suited to provide immediate value is at the point of care.
AI excels at reasoning over significant amounts of unstructured data. In healthcare, the amount of new data being produced significantly exceeds the time that doctors have to consume it – there are nearly 3,000 medical papers published every day and over 15 papers have been published by the time you’re done reading this blog. Put simply, we are in a golden age of drug discovery and that means our medical knowledge is doubling every 73 days.
But, despite this intense growth rate, the number of physicians isn’t keeping pace. Instead, we currently have a shortage of 64,000 physicians in the US and that number is only expected to worsen over the next few years. In other words, there is a clear mismatch in the rate of knowledge creation and consumption – while we have more medical information and data than ever, we also have a shortage of physicians to actually process that information. This means that physicians can no longer use the latest research to provide the best care to patients.
Fortunately, this task – synthesizing and reasoning over data across multiple sources – is exactly where AI excels. Unfortunately, AI also has a reliability problem. As I wrote about in the last edition, there are lots of challenges with red-teaming AI models and hallucinations still remain a big problem, especially for conversations that require long context windows.
These hallucinations are especially problematic in healthcare. Physicians have an incredibly high standard when adopting tools that support the point of care process: 100% accuracy is a requirement, not a nice to have. As a result, the tolerance for hallucinations is zero. This means that despite AI’s potential to help doctors provide better care, today’s large-scale, general foundation models aren’t suited for this.
But, smaller, healthcare-specific AI models trained exclusively on medical journals and peer-reviewed data can be. By building a model that isn’t trained on the internet but instead relies on RAG using pre-existing evidence sources, you can prevent inaccurate outputs and hallucinations. This model can therefore be used to provide physicians with the latest research, becoming a key part of their workflow at the point of care.
And from there, the path to expanding into other front and back office workflows is clear. Just like AI coding tools started by simply generating code and now they take the next step to run that code, a similar path exists here. Once physicians use a chat tool to assist them at the point of care, their next natural instinct will be to ask that AI copilot to actually take action. That next action could be anything from assisting with the claim submission process to helping with post-care communication, opening the door for this tool to expand beyond a simple knowledge acquisition model and actually solve the inefficiencies in the back office too.
This exact product – an AI copilot that enables physicians to get verified medical information that helps them make high-stake clinical decisions at the point of care – is exactly what OpenEvidence is building and it’s why I’ve chosen to cover them in this edition of “Startups to Join”. It’s also why 25% of US doctors are already using the platform and why Sequoia – who just led their $75M Series A – described them as “perhaps the fastest-growing healthcare business in history”.
OpenEvidence
At its core, OpenEvidence is an AI copilot trained using specialized medical content via licensing agreements they’ve established with leading journals like The New England Journal of Medicine. When a physician asks a question, the model searches a database of 35 million peer-reviewed publications to identify a conclusive answer. This approach means that OpenEvidence doesn’t hallucinate as it’s not trained on the inaccurate healthcare information that exists all over the internet.
Importantly, the responses are tailored to healthcare professionals. They use medical terminology, cite journal references, and provide potential follow-up questions to ensure every potential edge case is covered. And if you go onto the website and ask OpenEvidence a question, you’ll immediately notice a difference in the quality of output compared to general foundational models.
This difference in quality is also backed up by quantitative studies. General-purpose LLMs produce actionable responses (“of sufficient quality to justify or change clinical practice”) to clinical questions anywhere between 2-4% of the time. In contrast, OpenEvidence produces actionable responses 30% of the time.
Today, OpenEvidence is positioned to be a tool for physicians, not patients. While you can go onto the website and ask a few questions, you’ll eventually be asked to create an account and that requires an NIH number. This approach, alongside their free-to-use model subsidized by ad revenue, shows how OpenEvidence is effectively a healthcare business disguised as a consumer internet company – adoption is easy which makes the product incredibly sticky as they can provide immediate value with no implementation costs.
And this is a large part of why they’ve been so successful at achieving distribution. With over 35,000 physicians signing up every month, they’re on track to have 50% of US doctors signed up onto their platform by the end of the year. These users are also asking a lot of questions, with more than 2 million queries being answered by OpenEvidence in November alone. In other words, OpenEvidence is already improving millions of patient’s lives and their healthcare outcomes, while supporting overworked physicians in the golden age of medical discovery.
Concluding Thoughts + Jobs at OpenEvidence
While there still exist many challenges ahead, including the increasing number of inaccurate papers being published and the difficulties of expanding beyond the front office, by improving patient outcomes significantly and building trust with physicians around the country, OpenEvidence has already opened the door to tackle some of the biggest inefficiencies that exist across US healthcare today. And if joining the team to work on some of the biggest challenges in healthcare sounds exciting to you, they are actively hiring engineers – send over an email with a few sentences about yourself to engineering@openevidence.com :)
Resources
https://www.sequoiacap.com/article/partnering-with-openevidence-a-life-saving-healthcare-revolution/
https://arxiv.org/abs/2407.00541
https://www.forbes.com/sites/spencerdorn/2024/12/13/how-ai-is-changing-how-doctors-access-medical-knowledge/
https://timmermanreport.com/2024/10/and-just-like-that-what-the-viral-adoption-of-a-clinical-ai-app-means-for-pharma-rd/
https://www.reddit.com/r/medicine/comments/1dehwb3/we_are_openevidence_lets_talk_about_ai_and_llms/